Abstract

Introduction: The optimal duration of extended oral anticoagulant treatment for patients with venous thromboembolism (VTE) beyond the initial 3 to 6 months of the treatment remains undetermined. Group-based trajectory modeling (GBTM) is a data-driven method that can categorize patients with similar longitudinal adherence patterns over time into distinct subgroups. This study identified distinct patient subgroups with similar adherence trajectories of extended treatment of direct-acting oral anticoagulants (DOACs), and then examined the association between adherence trajectories and the risk of recurrent VTE and major bleeding among patients with VTE.
Methods: We identified patients ≥18 years with a diagnosis of deep vein thrombosis (DVT) or pulmonary embolism (PE) from inpatient claims using 2013-2019 Truven Commercial and Medicare Supplemental database. Patients were included if they initiated anticoagulants within 30 days of their first VTE diagnosis, completed 6 months of therapy-defined as ≥83% proportion days covered (PDC) with oral anticoagulants during the initial 6-month treatment period, and had extended treatment with any DOACs or no extended therapy. Based on the monthly PDC as the DOAC adherence measure, we used GBTM to identify DOAC adherence trajectories during 6 months of the extended treatment. The final trajectory model was chosen by assessing the Bayesian information criteria, Nagin's criteria, and having at least 10% of patients in each trajectory group for improving clinical utility. We compared recurrent VTE and major bleeding among adherence trajectory subgroups. Patients were followed up from the initiation of the extended treatment until the occurrence of the study outcomes, discontinuation of DOACs, switching to warfarin, end of study period, or end of enrollment, whichever occurred first. Cox proportional hazard modeling with inverse probability treatment weighting (IPTW) was used to obtain hazard ratios (HR) and 95% confidence intervals (95% CI).
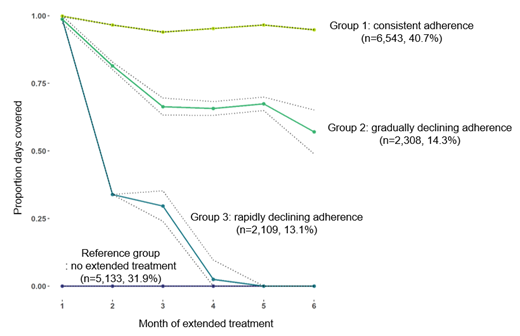
Results: The study cohort (mean age=58.7 years and 51.1% males) consisted of 10,960 patients with extended treatment of DOACs (4,294 apixaban, 6,409 rivaroxaban, 238 dabigatran, and 19 edoxaban users) with a mean treatment duration of 7.7 months and 5,133 patients with no extended treatment following completion of an initial 6 months of anticoagulant treatment. The final GBTM models identified four distinct adherence trajectories for extended therapy including (1) patients with consistent adherence (group 1, 40.7%), (2) patients with gradually declining adherence (group 2, 14.3%), (3) patients with rapidly declining adherence (group 3, 13.1%), and (4) patients with no extended treatment (reference group, 31.9%) (Figure 1). The incidence rates of recurrent VTE were 18.6, 46.9, 84.1, and 160.7 per 10,000 person-years, and those of major bleeding were 61.0, 125.1, 168.3, and 48.7 per 10,000 person-years in group 1, group 2, group 3, and the reference group, respectively. After IPTW, demographics and clinical characteristics (e.g., HAS-BLED bleeding risk score, provoked VTE) were comparable across the four trajectory groups with <0.1 of the standardized mean difference for each pairwise comparison. Compared to the reference group, group 1 (HR=0.09, 95% CI=0.05-0.17) and group 2 (HR=0.16, 95% CI=0.04-0.58) had decreased risk of recurrent VTE without increasing risk of major bleeding (HR=1.26, 95% CI=0.76-2.10 in group 1, HR=2.28, 95% CI=0.96-5.36 in group 2). There was no difference in the risk of recurrent VTE (HR=0.32, 95% CI=0.09-1.16) in group 3 but they had an increased risk of major bleeding (HR=2.69, 95% CI=1.00-7.23). The findings were consistent across different types of DOACs, suggesting a class effect of DOACs as extended therapy.
Conclusions: We identified 4 distinct trajectories of DOAC adherence during the 6 months of extended therapy among patients who completed 6 months of initial treatment. Compared to no extended treatment, persistent use of DOACs during extended treatment was associated with a lower risk of recurrent VTE without increasing major bleeding risk, whereas a rapid decline in adherence was associated with an increased risk of major bleeding with no difference in the risk of recurrence. Our findings provide evidence on the benefits of continuing and being adherent to extended anticoagulant treatment in patients with VTE without increasing the risk of major bleeding.
Kang: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding. Jones: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding. Lo-Ciganic: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding; MERCK: Research Funding. DeRemer: BMS advisory board attendee: Honoraria; Portola Pharmaceuticals: Current equity holder in publicly-traded company; BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding. Dietrich: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding. Huang: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding. Murphy: North American Thrombosis Foundation: Honoraria. Park: BMS/Pfizer Alliance American Thrombosis Investigator Initiated Research Program: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract